
Jun 21, 2016
New book on Human Computer Confluence - FREE PDF!
Two good news for Positive Technology followers.
1) Our new book on Human Computer Confluence is out!
2) It can be downloaded for free here

Human-computer confluence refers to an invisible, implicit, embodied or even implanted interaction between humans and system components. New classes of user interfaces are emerging that make use of several sensors and are able to adapt their physical properties to the current situational context of users.
A key aspect of human-computer confluence is its potential for transforming human experience in the sense of bending, breaking and blending the barriers between the real, the virtual and the augmented, to allow users to experience their body and their world in new ways. Research on Presence, Embodiment and Brain-Computer Interface is already exploring these boundaries and asking questions such as: Can we seamlessly move between the virtual and the real? Can we assimilate fundamentally new senses through confluence?
The aim of this book is to explore the boundaries and intersections of the multidisciplinary field of HCC and discuss its potential applications in different domains, including healthcare, education, training and even arts.
DOWNLOAD THE FULL BOOK HERE AS OPEN ACCESS
Please cite as follows:
Andrea Gaggioli, Alois Ferscha, Giuseppe Riva, Stephen Dunne, Isabell Viaud-Delmon (2016). Human computer confluence: transforming human experience through symbiotic technologies. Warsaw: De Gruyter. ISBN 9783110471120.
09:53 Posted in AI & robotics, Augmented/mixed reality, Biofeedback & neurofeedback, Blue sky, Brain training & cognitive enhancement, Brain-computer interface, Cognitive Informatics, Cyberart, Cybertherapy, Emotional computing, Enactive interfaces, Future interfaces, ICT and complexity, Neurotechnology & neuroinformatics, Positive Technology events, Research tools, Self-Tracking, Serious games, Technology & spirituality, Telepresence & virtual presence, Virtual worlds, Wearable & mobile | Permalink
Dec 26, 2015
How to reduce costs in Cyberpsychology research
Cyberpsychology is a fascinating field of research, yet it requires a lot of financial resources for its advancement. As an inherently interdisciplinary endeavor, the implementation of a cyberpsychology study often involves the collaboration of several scientific disciplines outside psychology, such as experts in human-computer interaction, software developers, data scientists, and engineers. Further, an increasing number of cyberpsychology studies consist of clinical trials, which can last several months (or even years) and involve a significant investment of economic resources. On the other side, finding adequate fundings is becoming the most pressing challenge for most cyberpsychologists.
This is due to several factors. First, governments university funding has fallen dramatically in most countries and the trend for the next years is not encouraging. Second, competition for grants is very high and it is likely to remain so. A third, - and perhaps less obvious - factor is that Cyberpsychology research tends to attract less fundings than other allied disciplines, i.e. medicine. Given this situation, what can be done to allow cyberpsychologists to keep furthering their research?
A possible strategy is to improve “lateral thinking” and find a way to optimize costs. This can be done, for example, by taking advantage of free, open source software/service/tools to support the different phases of the research process – design, implementation, collaboration, monitoring, data analysis, reporting, etc. These open-source tools are not only free, but sometimes even more powerful than existing proprietary software and services. For example, a fairly comprehensive set of free office productivity tools can be found online. These include word processor, spreadsheet (i.e. the OpenOffice suite), slide presentations, graphic programs (i.e. Gimp, http://www.gimp.org/).
As concerns the implementation of laboratory experiments, several software platforms are available for programming psychological studies. For example, PsychoPy is a user-friendly open-source application that allows the presentation of stimuli and collection of data for a wide range of neuroscience, psychology and psychophysics experiments. For the analysis of data, possible alternatives to commercial statistical packages include the R language for statistical computing, a free software environment for statistical computing and graphics (coupled with R-Commander or Rstudio for those who are not comfortable with line-command interfaces). And when it is time to writing a paper, free tools exist designed for the production of technical and scientific documentation, such as the popular program LaTeX, which can be used in combination to reference manager software like JabRef.
And what about Virtual Reality? Our NeuroVR platform is a free tool that young researchers (i.e. MS students, PhD students) can use to move their first scientific steps in the virtual realm.
Needless to say, the most expensive budget item in a research plan remains personnel costs. However, I think that by having a look at the many free scientific tools, resources and services that are available, it might be possible to significantly reduce the costs; at the same time, this approach offers the opportunity to support the growth of the open source community in our discipline.
11:24 Posted in Cybertherapy, Research tools | Permalink | Comments (0)
Apr 05, 2015
LED therapy for neurorehabilitation
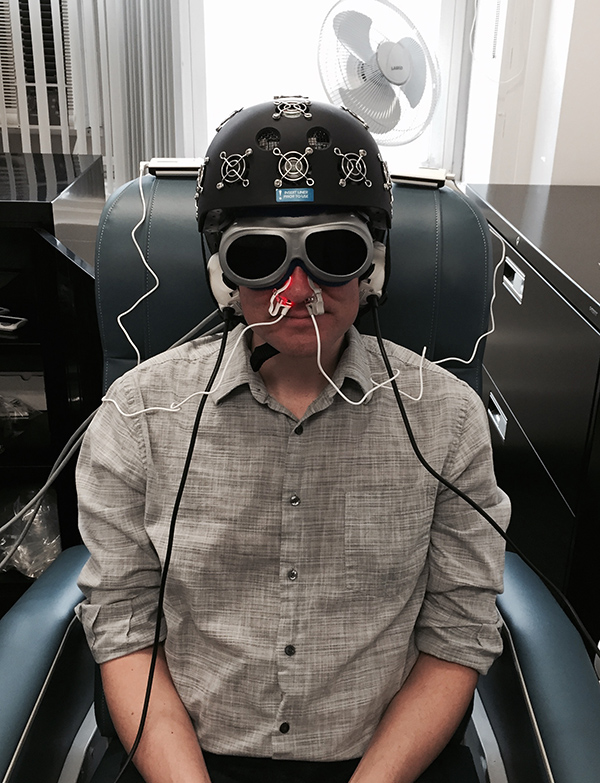
A staffer in Dr. Margaret Naeser’s lab demonstrates the equipment built especially for the research: an LED helmet (Photomedex), intranasal diodes (Vielight), and LED cluster heads placed on the ears (MedX Health). The real and sham devices look identical. Goggles are worn to block out the red light to avoid experimental artifacts. The near-infrared light is beyond the visible spectrum and cannot be seen. (credit: Naeser lab)
Researchers at the VA Boston Healthcare System are testing the effects of light therapy on brain function in the Veterans with Gulf War Illness study.
Veterans in the study wear a helmet lined with light-emitting diodes that apply red and near-infrared light to the scalp. They also have diodes placed in their nostrils, to deliver photons to the deeper parts of the brain.
The light is painless and generates no heat. A treatment takes about 30 minutes.
The therapy, though still considered “investigational” and not covered by most health insurance plans, is already used by some alternative medicine practitioners to treat wounds and pain.
The light from the diodes has been shown to boost the output of nitric oxide near where the LEDs are placed, which improves blood flow in that location.
“We are applying a technology that’s been around for a while,” says lead investigator Dr. Margaret Naeser, “but it’s always been used on the body, for wound healing and to treat muscle aches and pains, and joint problems. We’re starting to use it on the brain.”
Naeser is a research linguist and speech pathologist for the Boston VA, and a research professor of neurology at Boston University School of Medicine (BUSM).
How LED therapy works
The LED therapy increases blood flow in the brain, as shown on MRI scans. It also appears to have an effect on damaged brain cells, specifically on their mitochondria. These are bean-shaped subunits within the cell that put out energy in the form of a chemical known as ATP. The red (600 nm) and NIR (800–900nm) wavelengths penetrate through the scalp and skull by about 1 cm to reach brain cells and spur the mitochondria to produce more ATP. That can mean clearer, sharper thinking, says Naeser.
Nitric oxide is also released and diffused outside the cell wall, promoting local vasodilation and increased blood flow.
Naeser says brain damage caused by explosions, or exposure to pesticides or other neurotoxins — such as in the Gulf War — could impair the mitochondria in cells. She believes light therapy can be a valuable adjunct to standard cognitive rehabilitation, which typically involves “exercising” the brain in various ways to take advantage of brain plasticity and forge new neural networks.
“The light-emitting diodes add something beyond what’s currently available with cognitive rehabilitation therapy,” says Naeser. “That’s a very important therapy, but patients can go only so far with it. And in fact, most of the traumatic brain injury and PTSD cases that we’ve helped so far with LEDs on the head have been through cognitive rehabilitation therapy. These people still showed additional progress after the LED treatments. It’s likely a combination of both methods would produce the best results.”
Results published from 11 TBI patients
The LED approach has its skeptics, but Naeser’s group has already published some encouraging results in the peer-reviewed scientific literature.
Last June in the Journal of Neurotrauma, they reported in an open-access paper, the outcomes of LED therapy in 11 patients with chronic TBI, ranging in age from 26 to 62. Most of the injuries occurred in car accidents or on the athletic field. One was a battlefield injury, from an improvised explosive device (IED).
Neuropsychological testing before the therapy and at several points thereafter showed gains in areas such as executive function, verbal learning, and memory. The study volunteers also reported better sleep and fewer PTSD symptoms.
The study authors concluded that the pilot results warranted a randomized, placebo-controlled trial — the gold standard in medical research.
That’s happening now, thanks to VA support. One trial, already underway, aims to enroll 160 Gulf War veterans. Half the veterans will get the real LED therapy for 15 sessions, while the others will get a mock version, using sham lights.
Then the groups will switch, so all the volunteers will end up getting the real therapy, although they won’t know at which point they received it. After each Veteran’s last real or sham treatment, he or she will undergo tests of brain function.
Naeser points out that “because this is a blinded, controlled study, neither the participant nor the assistant applying the LED helmet and the intranasal diodes is aware whether the LEDs are real or sham — they both wear goggles that block out the red LED light.” The near-infrared light is invisible.
Upcoming trials
Other trials of the LED therapy are getting underway:
- Later this year, a trial will launch for Veterans age 18 to 55 who have both traumatic brain injury (TBI) and post-traumatic stress disorder, a common combination in recent war Veterans. The VA-funded study will be led by Naeser’s colleague Dr. Jeffrey Knight, a psychologist with VA’s National Center for PTSD and an assistant professor of psychiatry at BUSM.
- Dr. Yelena Bogdanova, a clinical psychologist with VA and assistant professor of psychiatry at BUSM, will lead a VA-funded trial looking at the impact of LED therapy on sleep and cognition in Veterans with blast TBI.
- Naeser is collaborating on an Army study testing LED therapy, delivered via the helmets and the nose diodes, for active-duty soldiers with blast TBI. The study, funded by the Army’s Advanced Medical Technology Initiative, will also test the feasibility and effectiveness of using only the nasal LED devices — and not the helmets — as an at-home, self-administered treatment. The study leader is Dr. Carole Palumbo, an investigator with VA and the Army Research Institute of Environmental Medicine, and an associate professor of neurology at BUSM.
Naeser hopes the work will validate LED therapy as a viable treatment for veterans and others with brain difficulties. She also foresees potential for conditions such as depression, stroke, dementia, and even autism.
According to sources cited by the authors, i is estimated that there are 5,300,000 Americans living with TBI-related disabilities. The annual economic cost is estimated to be between $60 and $76.5 billion. It is estimated that 15–40% of soldiers returning from Iraq and Afghanistan as part of Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF) report at least one TBI. And within the past 10 years, the diagnosis of concussion in high school sports has increased annually by 16.5%.
The research was supported by U.S. Department of Veterans Affairs. National Institutes of Health, American Medical Society for Sports Medicine, and American College of Sports Medicine-American Medical Society for Sports Medicine Foundation.
22:59 Posted in Brain training & cognitive enhancement, Cybertherapy | Permalink | Comments (0)
Aug 03, 2014
Detecting awareness in patients with disorders of consciousness using a hybrid brain-computer interface
Detecting awareness in patients with disorders of consciousness using a hybrid brain-computer interface.
J Neural Eng. 2014 Aug 1;11(5):056007
Authors: Pan J, Xie Q, He Y, Wang F, Di H, Laureys S, Yu R, Li Y
Abstract. Objective. The bedside detection of potential awareness in patients with disorders of consciousness (DOC) currently relies only on behavioral observations and tests; however, the misdiagnosis rates in this patient group are historically relatively high. In this study, we proposed a visual hybrid brain-computer interface (BCI) combining P300 and steady-state evoked potential (SSVEP) responses to detect awareness in severely brain injured patients. Approach. Four healthy subjects, seven DOC patients who were in a vegetative state (VS, n = 4) or minimally conscious state (MCS, n = 3), and one locked-in syndrome (LIS) patient attempted a command-following experiment. In each experimental trial, two photos were presented to each patient; one was the patient's own photo, and the other photo was unfamiliar. The patients were instructed to focus on their own or the unfamiliar photos. The BCI system determined which photo the patient focused on with both P300 and SSVEP detections. Main results. Four healthy subjects, one of the 4 VS, one of the 3 MCS, and the LIS patient were able to selectively attend to their own or the unfamiliar photos (classification accuracy, 66-100%). Two additional patients (one VS and one MCS) failed to attend the unfamiliar photo (50-52%) but achieved significant accuracies for their own photo (64-68%). All other patients failed to show any significant response to commands (46-55%). Significance. Through the hybrid BCI system, command following was detected in four healthy subjects, two of 7 DOC patients, and one LIS patient. We suggest that the hybrid BCI system could be used as a supportive bedside tool to detect awareness in patients with DOC.
22:34 Posted in Brain-computer interface, Cybertherapy, Research tools | Permalink | Comments (0)
Jul 30, 2014
A virtual rehabilitation program after amputation: a phenomenological exploration
A virtual rehabilitation program after amputation: a phenomenological exploration.
Disabil Rehabil Assist Technol. 2013 Nov;8(6):511-5
Authors: Moraal M, Slatman J, Pieters T, Mert A, Widdershoven G
Abstract. PURPOSE: This study provides an analysis of bodily experiences of a man with a lower leg amputation who used a virtual rehabilitation program. METHOD: The study reports data from semi-structured interviews with a 32-year veteran who used a virtual environment during rehabilitation. The interviews were analyzed using interpretative phenomenological analysis (IPA). RESULTS: During this rehabilitation program, he initially experienced his body as an object, which he had to handle carefully. As he went along with the training sessions, however, he was more stimulated to react directly without being aware of the body's position. In order to allow himself to react spontaneously, he needed to gain trust in the device. This was fostered by his narrative, in which he stressed how the device mechanically interacts with his movements. CONCLUSION: The use of a virtual environment facilitated the process of re-inserting one's body into the flow of one's experience in two opposite, but complementary ways: (1) it invited this person to move automatically without taking into account his body; (2) it invited him to take an instrumental or rational view on his body. Both processes fostered his trust in the device, and ultimately in his body. IMPLICATIONS FOR REHABILITATION: Providing (more) technological explanation of the technological device (i.e. the virtual environment), may facilitate a rehabilitation process. Providing (more) explicit technological feedback, during training sessions in a virtual environment, may facilitate a rehabilitation process.
21:37 Posted in Cybertherapy, Virtual worlds | Permalink | Comments (0)
Characteristics of Successful Technological Interventions in Mental Resilience Training
Characteristics of Successful Technological Interventions in Mental Resilience Training.
J Med Syst. 2014 Sep;38(9):113
Authors: Vakili V, Brinkman WP, Morina N, Neerincx MA
Abstract. In the last two decades, several effective virtual reality-based interventions for anxiety disorders have been developed. Virtual reality interventions can also be used to build resilience to psychopathology for populations at risk of exposure to traumatic experiences and developing mental disorders as a result, such as for people working in vulnerable professions. Despite the interest among mental health professionals and researchers in applying new technology-supported interventions for pre-trauma mental resilience training, there is a lack of recommendations about what constitutes potentially effective technology-supported resilience training. This article analyses the role of technology in the field of stress-resilience training. It presents lessons learned from technology developers currently working in the area, and it identifies some key clinical requirements for the supported resilience interventions. Two processes made up this research: 1) developers of technology-assisted resilience programs were interviewed regarding human-computer interaction and system development; 2) discussions with clinicians were prompted using technology-centered concept storyboards to elicit feedback, and to refine, validate and extend the initial concepts. A qualitative analysis of the interviews produced a set of development guidelines that engineers should follow and a list of intervention requirements that the technology should fulfill. These recommendations can help bridge the gap between engineers and clinicians when generating novel resilience interventions for people in vulnerable professions.
21:35 Posted in Cybertherapy | Permalink | Comments (0)
Jul 29, 2014
Ekso bionic suit
Ekso is an exoskeleton bionic suit or a "wearable robot" designed to enable individuals with lower extremity paralysis to stand up and walk over ground with a weight bearing, four point reciprocal gait. Walking is achieved by the user’s forward lateral weight shift to initiate a step. Battery-powered motors drive the legs and replace neuromuscular function.
Ekso Bionics http://eksobionics.com/
14:59 Posted in AI & robotics, Cybertherapy, Wearable & mobile | Permalink | Comments (0)
Jul 09, 2014
Experiential Virtual Scenarios With Real-Time Monitoring (Interreality) for the Management of Psychological Stress: A Block Randomized Controlled Trial
The recent convergence between technology and medicine is offering innovative methods and tools for behavioral health care. Among these, an emerging approach is the use of virtual reality (VR) within exposure-based protocols for anxiety disorders, and in particular posttraumatic stress disorder. However, no systematically tested VR protocols are available for the management of psychological stress. Objective: Our goal was to evaluate the efficacy of a new technological paradigm, Interreality, for the management and prevention of psychological stress. The main feature of Interreality is a twofold link between the virtual and the real world achieved through experiential virtual scenarios (fully controlled by the therapist, used to learn coping skills and improve self-efficacy) with real-time monitoring and support (identifying critical situations and assessing clinical change) using advanced technologies (virtual worlds, wearable biosensors, and smartphones).
Full text paper available at: http://www.jmir.org/2014/7/e167/
Apr 29, 2014
Evidence, Enactment, Engagement: The three 'nEEEds' of mental mHealth
Actually, according to my experience, citizens and public stakeholders are not well-informed or educated about mHealth. For example, to many people the idea of using phones to deliver mental health programs still sounds weird.
Yet the number of mental health apps is rapidly growing: a recent survey identified 200 unique mobile tools specifically associated with behavioral health.
These applications now cover a wide array of clinical areas including developmental disorders, cognitive disorders, substance-related disorders, as well as psychotic and mood disorders.
I think that the increasing "applification" of mental health is explained by three potential benefits of this approach:
- First, mobile apps can be integrated in different stages of treatment: from promoting awareness of disease, to increasing treatment compliance, to preventing relapse.
- Furthermore, mobile tools can be used to monitor behavioural and psychological symptoms in everyday life: self-reported data can be complemented with readings from inbuilt or wearable sensors to fine-tune treatment according to the individual patient’s needs.
- Last - but not least - mobile applications can help patients to stay on top of current research, facilitating access to evidence-based care. For example, in the EC-funded INTERSTRESS project, we investigated these potentials in the assessment and management of psychological stress, by developing different mobile applications (including the award-winning Positive Technology app) for helping people to monitor stress levels “on the go” and learn new relaxation skills.
In short, I believe that mental mHealth has the potential to provide the right care, at the right time, at the right place. However, from my personal experience I have identified three key challenges that must be faced in order to realize the potential of this approach.
I call them the three "nEEEds" of mental mHealth: evidence, engagement, enactment.
- Evidence refers to the need of clinical proof of efficacy or effectiveness to be provided using randomised trials.
- Engagement is related to the need of ensuring usability and accessibility for mobile interfaces: this goes beyond reducing use errors that may generate risks of psychological discomfort for the patient, to include the creation of a compelling and engaging user experience.
- Finally, enactment concerns the need that appropriate regulations enacted by competent authorities catch up with mHealth technology development.
Being myself a beneficiary of EC-funded grants, I can recognize that R&D investments on mHealth made by EC across FP6 and FP7 have contributed to position Europe at the forefront of this revolution. And the return of this investment could be strong: it has been predicted that full exploitation of mHealth solutions could lead to nearly 100 billion EUR savings in total annual EU healthcare spend in 2017.
I believe that a progressively larger portion of these savings may be generated by the adoption of mobile solutions in the mental health sector: actually, in the WHO European Region, mental ill health accounts for almost 20% of the burden of disease.
For this prediction to be fulfilled, however, many barriers must be overcome: thethree "nEEEds" of mental mHealth are probably only the start of the list. Hopefully, the Green Paper consultation will help to identify further opportunities and concerns that may be facing mental mHealth, in order to ensure a successful implementation of this approach.
23:51 Posted in Cybertherapy, Physiological Computing, Wearable & mobile | Permalink | Comments (0)
Apr 15, 2014
A post-stroke rehabilitation system integrating robotics, VR and high-resolution EEG imaging
A post-stroke rehabilitation system integrating robotics, VR and high-resolution EEG imaging.
IEEE Trans Neural Syst Rehabil Eng. 2013 Sep;21(5):849-59
Authors: Steinisch M, Tana MG, Comani S
Abstract
We propose a system for the neuro-motor rehabilitation of upper limbs in stroke survivors. The system is composed of a passive robotic device (Trackhold) for kinematic tracking and gravity compensation, five dedicated virtual reality (VR) applications for training of distinct movement patterns, and high-resolution EEG for synchronous monitoring of cortical activity. In contrast to active devices, the Trackhold omits actuators for increased patient safety and acceptance levels, and for reduced complexity and costs. VR applications present all relevant information for task execution as easy-to-understand graphics that do not need any written or verbal instructions. High-resolution electroencephalography (HR-EEG) is synchronized with kinematic data acquisition, allowing for the epoching of EEG signals on the basis of movement-related temporal events. Two healthy volunteers participated in a feasibility study and performed a protocol suggested for the rehabilitation of post-stroke patients. Kinematic data were analyzed by means of in-house code. Open source packages (EEGLAB, SPM, and GMAC) and in-house code were used to process the neurological data. Results from kinematic and EEG data analysis are in line with knowledge from currently available literature and theoretical predictions, and demonstrate the feasibility and potential usefulness of the proposed rehabilitation system to monitor neuro-motor recovery.
23:16 Posted in Cybertherapy, Virtual worlds | Permalink | Comments (0)
Apr 06, 2014
The effects of augmented visual feedback during balance training in Parkinson's disease - trial protocol
The effects of augmented visual feedback during balance training in Parkinson's disease: study design of a randomized clinical trial.
BMC Neurol. 2013;13:137
Authors: van den Heuvel MR, van Wegen EE, de Goede CJ, Burgers-Bots IA, Beek PJ, Daffertshofer A, Kwakkel G
Abstract. BACKGROUND: Patients with Parkinson's disease often suffer from reduced mobility due to impaired postural control. Balance exercises form an integral part of rehabilitative therapy but the effectiveness of existing interventions is limited. Recent technological advances allow for providing enhanced visual feedback in the context of computer games, which provide an attractive alternative to conventional therapy. The objective of this randomized clinical trial is to investigate whether a training program capitalizing on virtual-reality-based visual feedback is more effective than an equally-dosed conventional training in improving standing balance performance in patients with Parkinson's disease.
METHODS/DESIGN: Patients with idiopathic Parkinson's disease will participate in a five-week balance training program comprising ten treatment sessions of 60 minutes each. Participants will be randomly allocated to (1) an experimental group that will receive balance training using augmented visual feedback, or (2) a control group that will receive balance training in accordance with current physical therapy guidelines for Parkinson's disease patients. Training sessions consist of task-specific exercises that are organized as a series of workstations. Assessments will take place before training, at six weeks, and at twelve weeks follow-up. The functional reach test will serve as the primary outcome measure supplemented by comprehensive assessments of functional balance, posturography, and electroencephalography. DISCUSSION: We hypothesize that balance training based on visual feedback will show greater improvements on standing balance performance than conventional balance training. In addition, we expect that learning new control strategies will be visible in the co-registered posturographic recordings but also through changes in functional connectivity.
23:35 Posted in Augmented/mixed reality, Cybertherapy | Permalink | Comments (0)
Mar 03, 2014
Virtual reality for the assessment of frontotemporal dementia, a feasibility study
Virtual reality for the assessment of frontotemporal dementia, a feasibility study.
Disabil Rehabil Assist Technol. 2014 Feb 14;
Authors: Mendez MF, Joshi A, Jimenez E
Abstract
Abstract Purpose: Behavioral variant frontotemporal dementia (bvFTD) is a non-Alzheimer dementia characterized by difficulty in documenting social-emotional changes. Few investigations have used virtual reality (VR) for documentation and rehabilitation of non-Alzheimer dementias. Methods: Five bvFTD patients underwent insight interviews while immersed in a virtual environment. They were interviewed by avatars, their answers were recorded, and their heart rates were monitored. They were asked to give ratings of their stress immediately at the beginning and at the end of the session. Results: The patients tolerated the head-mounted display and VR without nausea or disorientation, heart rate changes, or worsening stress ratings. Their insight responses were comparable to real world interviews. All bvFTD patients showed their presence in the VR environment as they moved their heads to face and respond to each avatar's questions. The bvFTD patients tended to greater verbal elaboration of answers with larger mean length of utterances compared to their real world interviews. Conclusions: VR is feasible and well-tolerated in bvFTD. These patients may have VR responses comparable to real world performance and they may display a presence in the virtual environment which could even facilitate assessment. Further research can explore the promise of VR for the evaluation and rehabilitation of dementias beyond Alzheimer's disease. Implications for Rehabilitation Clinicians need effective evaluation and rehabilitation strategies for dementia, a neurological syndrome of epidemic proportions and a leading cause of disability. Memory and cognitive deficits are the major disabilities and targets for rehabilitation in Alzheimer's disease, the most common dementia. In contrast, social and emotional disturbances are the major disabilities and targets for rehabilitation in behavioral variant frontotemporal dementia (bvFTD), an incompletely understood non-Alzheimer dementia. Virtual reality is a technology that holds great promise for the evaluation and rehabilitation of patients with bvFTD and other non-Alzheimer dementias, and preliminary evidence suggests that this technology is feasible in patients with bvFTD.
00:27 Posted in Cybertherapy, Virtual worlds | Permalink | Comments (0)
Evaluation of a virtual reality prospective memory task for use with individuals with severe traumatic brain injury
Evaluation of a virtual reality prospective memory task for use with individuals with severe traumatic brain injury.
Neuropsychol Rehabil. 2014 Feb 24;
Authors: Canty AL, Fleming J, Patterson F, Green HJ, Man D, Shum DH
Abstract
The current study aimed to evaluate the sensitivity, convergent validity and ecological validity of a newly developed virtual reality prospective memory (PM) task (i.e., the Virtual Reality Shopping Task; VRST) for use with individuals with traumatic brain injury (TBI). Thirty individuals with severe TBI and 24 uninjured adults matched on age, gender and education level were administered the VRST, a lexical decision PM task (LDPMT), an index of task-friendliness and a cognitive assessment battery. Significant others rated disruptions in the TBI participants' occupational activities, interpersonal relationships and independent living skills. The performance of the TBI group was significantly poorer than that of controls on event-based PM as measured by the LDPMT, and on time- and event-based PM as measured by the VRST. Performance on the VRST significantly predicted significant others' ratings of patients' occupational activities and independent living skills. The VRST was rated as significantly more reflective of an everyday activity, interesting and was afforded a higher recommendation than the LDPMT. For the TBI group, event and total PM performance on the VRST significantly correlated with performance on measures of mental flexibility and verbal fluency, and total PM performance correlated with verbal memory. These results provide preliminary but promising evidence of the sensitivity, as well as the convergent and ecological validity of the VRST.
00:23 Posted in Cybertherapy, Virtual worlds | Permalink | Comments (0)
Virtual Reality for sensorimotor rehabilitation post-stroke
Virtual Reality for Sensorimotor Rehabilitation Post-Stroke: The Promise and Current State of the Field.
Curr Phys Med Rehabil Reports. 2013 Mar;1(1):9-20
Authors: Fluet GG, Deutsch JE
Abstract
Developments over the past 2 years in virtual reality (VR) augmented sensorimotor rehabilitation of upper limb use and gait post-stroke were reviewed. Studies were included if they evaluated comparative efficacy between VR and standard of care, and or differences in VR delivery methods; and were CEBM (center for evidence based medicine) level 2 or higher. Eight upper limb and two gait studies were included and described using the following categories hardware (input and output), software (virtual task and feedback and presentation) intervention (progression and dose), and outcomes. Trends in the field were commented on, gaps in knowledge identified, and areas of future research and translation of VR to practice were suggested.
00:20 Posted in Cybertherapy, Virtual worlds | Permalink | Comments (0)
Mar 02, 2014
Myoelectric controlled avatar helps stop phantom limb pain
Reblogged from Medgadget
People unfortunate enough to lose an arm or a leg often feel pain in their missing limb, an unexplained condition known as phantom limb pain. Researchers at Chalmers University of Technology in Sweden decided to test whether they can fool the brain into believing the limb is still there and maybe stop the pain.
They attached electrodes to the skin of the remaining arm of an amputee to read the myoelectric signals from the muscles below. Additionally, the arm was tracked in 3D using a marker so that the data could be integrated into a moving generated avatar as well as computer games. The amputee moves the arm of the avatar like he would if his own still existed, while the brain becomes reacquainted with its presence. After repeated use, and playing video games that were controlled using the same myoelectric interface, the person in the study had significant pain reduction after decades of phantom limb pain.
Here’s a video showing off the experimental setup:
Study in Frontiers in Neuroscience: Treatment of phantom limb pain (PLP) based on augmented reality and gaming controlled by myoelectric pattern recognition: a case study of a chronic PLP patient…
22:35 Posted in Cybertherapy, Wearable & mobile | Permalink | Comments (0)
Feb 09, 2014
A high-fidelity virtual environment for the study of paranoia
A high-fidelity virtual environment for the study of paranoia.
Schizophr Res Treatment. 2013;2013:538185
Authors: Broome MR, Zányi E, Hamborg T, Selmanovic E, Czanner S, Birchwood M, Chalmers A, Singh SP
Abstract. Psychotic disorders carry social and economic costs for sufferers and society. Recent evidence highlights the risk posed by urban upbringing and social deprivation in the genesis of paranoia and psychosis. Evidence based psychological interventions are often not offered because of a lack of therapists. Virtual reality (VR) environments have been used to treat mental health problems. VR may be a way of understanding the aetiological processes in psychosis and increasing psychotherapeutic resources for its treatment. We developed a high-fidelity virtual reality scenario of an urban street scene to test the hypothesis that virtual urban exposure is able to generate paranoia to a comparable or greater extent than scenarios using indoor scenes. Participants (n = 32) entered the VR scenario for four minutes, after which time their degree of paranoid ideation was assessed. We demonstrated that the virtual reality scenario was able to elicit paranoia in a nonclinical, healthy group and that an urban scene was more likely to lead to higher levels of paranoia than a virtual indoor environment. We suggest that this study offers evidence to support the role of exposure to factors in the urban environment in the genesis and maintenance of psychotic experiences and symptoms. The realistic high-fidelity street scene scenario may offer a useful tool for therapists.
22:25 Posted in Cybertherapy, Research tools, Virtual worlds | Permalink | Comments (0)
Effects of the addition of transcranial direct current stimulation to virtual reality therapy after stroke: A pilot randomized controlled trial
Effects of the addition of transcranial direct current stimulation to virtual reality therapy after stroke: A pilot randomized controlled trial.
NeuroRehabilitation. 2014 Jan 28;
Authors: Viana RT, Laurentino GE, Souza RJ, Fonseca JB, Silva Filho EM, Dias SN, Teixeira-Salmela LF, Monte-Silva KK
Abstract. BACKGROUND: Upper limb (UL) impairment is the most common disabling deficit following a stroke. Previous studies have suggested that transcranial direct current stimulation (tDCS) enhances the effect of conventional therapies.
OBJECTIVE: This pilot double-blind randomized control trial aimed to determine whether or not tDCS, combined with Wii virtual reality therapy (VRT), would be superior to Wii therapy alone in improving upper limb function and quality of life in chronic stroke individuals.
METHODS: Twenty participants were randomly assigned either to an experimental group that received VRT and tDCS, or a control group that received VRT and sham tDCS. The therapy was delivered over 15 sessions with 13 minutes of active or sham anodal tDCS, and one hour of virtual reality therapy. The outcomes included were determined using the Fugl-Meyer scale, the Wolf motor function test, the modified Ashworth scale (MAS), grip strength, and the stroke specific quality of life scale (SSQOL). Minimal clinically important differences (MCID) were observed when assessing outcome data.
RESULTS: Both groups demonstrated gains in all evaluated areas, except for the SSQOL-UL domain. Differences between groups were only observed in wrist spasticity levels in the experimental group, where more than 50% of the participants achieved the MCID.
CONCLUSIONS: These findings support that tDCS, combined with VRT therapy, should be investigated and clarified further.
22:21 Posted in Brain stimulation, Cybertherapy, Virtual worlds | Permalink | Comments (0)
Dec 21, 2013
Effectiveness and feasibility of virtual reality and gaming system use at home by older adults
Effectiveness and feasibility of virtual reality and gaming system use at home by older adults for enabling physical activity to improve health-related domains: a systematic review.
Age Ageing. 2013 Dec 17; Authors: Miller KJ, Adair BS, Pearce AJ, Said CM, Ozanne E, Morris MM
BACKGROUND: use of virtual reality and commercial gaming systems (VR/gaming) at home by older adults is receiving attention as a means of enabling physical activity. OBJECTIVE: to summarise evidence for the effectiveness and feasibility of VR/gaming system utilisation by older adults at home for enabling physical activity to improve impairments, activity limitations or participation. METHODS: a systematic review searching 12 electronic databases from 1 January 2000-10 July 2012 using key search terms. Two independent reviewers screened yield articles using pre-determined selection criteria, extracted data using customised forms and applied the Cochrane Collaboration Risk of Bias Tool and the Downs and Black Checklist to rate study quality. RESULTS: fourteen studies investigating the effects of VR/gaming system use by healthy older adults and people with neurological conditions on activity limitations, body functions and physical impairments and cognitive and emotional well-being met the selection criteria. Study quality ratings were low and, therefore, evidence was not strong enough to conclude that interventions were effective. Feasibility was inconsistently reported in studies. Where feasibility was discussed, strong retention (≥70%) and adherence (≥64%) was reported. Initial assistance to use the technologies, and the need for monitoring exertion, aggravation of musculoskeletal symptoms and falls risk were reported. CONCLUSIONS: existing evidence to support the feasibility and effectiveness VR/gaming systems use by older adults at home to enable physical activity to address impairments, activity limitations and participation is weak with a high risk of bias. The findings of this review may inform future, more rigorous research.
20:11 Posted in Cybertherapy, Serious games, Virtual worlds | Permalink | Comments (0)
Nov 20, 2013
inFORM
inFORM is a Dynamic Shape Display developed by MIT Tangible Media Group that can render 3D content physically, so users can interact with digital information in a tangible way.
inFORM can also interact with the physical world around it, for example moving objects on the table’s surface.
Remote participants in a video conference can be displayed physically, allowing for a strong sense of presence and the ability to interact physically at a distance.
Nov 16, 2013
Neurofeedback training aimed to improve focused attention and alertness in children with ADHD
Neurofeedback training aimed to improve focused attention and alertness in children with ADHD: a study of relative power of EEG rhythms using custom-made software application.
Clin EEG Neurosci. 2013 Jul;44(3):193-202
Authors: Hillard B, El-Baz AS, Sears L, Tasman A, Sokhadze EM
Abstract. Neurofeedback is a nonpharmacological treatment for attention-deficit hyperactivity disorder (ADHD). We propose that operant conditioning of electroencephalogram (EEG) in neurofeedback training aimed to mitigate inattention and low arousal in ADHD, will be accompanied by changes in EEG bands' relative power. Patients were 18 children diagnosed with ADHD. The neurofeedback protocol ("Focus/Alertness" by Peak Achievement Trainer) has a focused attention and alertness training mode. The neurofeedback protocol provides one for Focus and one for Alertness. This does not allow for collecting information regarding changes in specific EEG bands (delta, theta, alpha, low and high beta, and gamma) power within the 2 to 45 Hz range. Quantitative EEG analysis was completed on each of twelve 25-minute-long sessions using a custom-made MatLab application to determine the relative power of each of the aforementioned EEG bands throughout each session, and from the first session to the last session. Additional statistical analysis determined significant changes in relative power within sessions (from minute 1 to minute 25) and between sessions (from session 1 to session 12). Analysis was of relative power of theta, alpha, low and high beta, theta/alpha, theta/beta, and theta/low beta and theta/high beta ratios. Additional secondary measures of patients' post-neurofeedback outcomes were assessed, using an audiovisual selective attention test (IVA + Plus) and behavioral evaluation scores from the Aberrant Behavior Checklist. Analysis of data computed in the MatLab application, determined that theta/low beta and theta/alpha ratios decreased significantly from session 1 to session 12, and from minute 1 to minute 25 within sessions. The findings regarding EEG changes resulting from brain wave self-regulation training, along with behavioral evaluations, will help elucidate neural mechanisms of neurofeedback aimed to improve focused attention and alertness in ADHD.
15:49 Posted in Biofeedback & neurofeedback, Cybertherapy | Permalink | Comments (0)






